Weakened immune system: risk of mutations in antibody therapy – know
Antibodies from recovering patients are a treatment option for Covid-19 – especially for patients with weakened immune systems. But doctors have long worried that mutations could develop well. If a person’s immune system is weakened by chemotherapy, for example, the immune system is barely able to successfully fight viruses. British researchers wrote in a recent article in the journal Nature: “The antibodies that are ingested are barely supported by cytotoxic T cells, which reduces the chances of eliminating the virus.” a study.
Then the infection often becomes chronic and there is an increased risk that the virus will mutate and develop variants with new characteristics. In the case of serum treatment upon contact with donor antibodies, it is particularly those variants against which these antibodies are less effective that they predominate. The effect can be similar in the case of insufficiently effective vaccination.
Over three months, 23 genome sequences
Researchers from the “Genomics UK” consortium had the opportunity to follow the relationship between chronic infection and mutations and serum therapy for a period of 101 days in an immunocompromised Covid patient. The British patient was over 70 years old and had a lymphatic tumor disease occurring in the mucous membranes. His immune system has been weakened by the chemotherapy. When he contracted SARS-CoV-2, he was initially treated with serum therapy, among other things. His condition initially stabilized, but then significantly deteriorated. Despite the extra treatment, he died. During those 101 days, 23 virus samples were taken and their genomes sequenced. This made it possible to see how the virus had mutated.
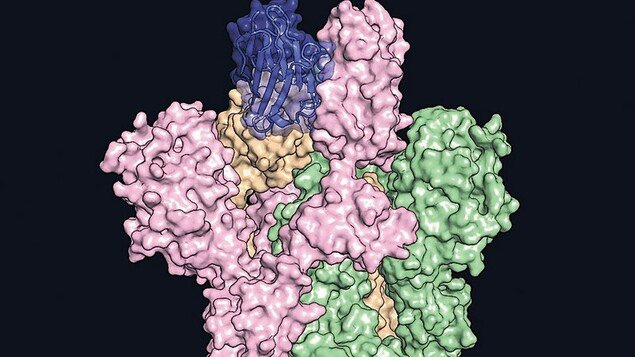
After two treatments with Antibody serum treatment The researchers observed the clearest change in the number of people infected with the virus between day 66 and 82. The type of virus that survived the antibody treatment became dominant. On the one hand, it contains the so-called double deletion by which two amino acids are lost in the protein.
An evolutionary race with a treatment effect
This change, called H69 / V70, is close to the spiny protein receptor binding site, which the virus uses as a key to invading cells. There’s also another nearby boom known as the D796H. Together, they both cause a structural change in the protein. It leads to the fact that the taken antibodies are more difficult to match and harder to neutralize the virus.
Initially, this variable virus took a back seat, but after the third round of treatment it saw another spike in numbers. “What we saw was basically a competition between different types of viruses and we think that competition is fueled by serum therapy,” said one of the study authors, Ravi Gupta of the Cambridge Institute for Therapeutic Immunology and Infectious Diseases.
In people with a normal immune system, the virus is not expected to mutate as a result of serum therapy as it is in immunocompromised patients. Because in these cases, the antibodies are adequately supported by cytotoxic T cells in the immune system. It can recognize and eliminate infected cells. Together, the antibodies and cytotoxic T cells have a greater ability to stop viruses.
Isolate patients as best as possible
By using industrially produced viruses containing either the H69 / V70 deletion, the D796 mutation, or both at the same time, British scientists have succeeded in determining the cause of the mutations. In laboratory experiments without antibodies, deletion alone doubled virus infection compared to the old virus. It is also important that the deletion of the H69 / V70 also occurs in the “British” variant B.1.1.7.
In contrast, D796H is the so-called escape mutation. Here the receptor binding site is altered so that the antibodies from healthy Covid 19 patients cannot catch the virus there either. This reduces the effectiveness of the serum therapy. “Given that both vaccines and therapies target the spike protein that has been mutated in our patient, our study makes the most worrisome option for the virus to outpace vaccines by mutating appropriately,” says Ravi Gupta.
However, “it is unlikely that this formation of virus variants will occur in patients with an active immune system, as fewer viral variants could arise due to better immune control.” But the serum treatment enhanced the selection of virus variants that are less sensitive or insensitive to antibodies in this and at least one other patient with immunodeficiency in the USA. “It shows how careful we should be when treating immunocompromised patients who have more time to reproduce, which means it also has more opportunities to mutate,” the study authors wrote.
Limited use
As long as more data are not available, the researchers recommend that serum treatment of immunocompromised patients should only be conducted as part of studies and preferably in single rooms with increased infection control precautions due to the increased risk of viral mutations. Special effort must be made to prevent injury to others. Continuous sequencing of the virus is also required.
It is also now known that serum therapies are only successful under certain conditions, even in Covid-19 patients who are not immunocompromised. This is why the US Food and Drug Administration (FDA) has restricted its use now: In the future, it should only be used in the early phase of treatment, that is, in the first 72 hours, and in patients whose immune cells do not produce enough antibodies for defense.

“Organizer. Social media geek. General communicator. Bacon scholar. Proud pop culture trailblazer.”
